In a plenary session delivered at the Alzheimer’s Association International Conference (AAIC) 2017, held in London, United Kingdom, Julie Williams, Ph.D. – a professor in the Division of Psychological Medicine and Clinical Neurosciences at Cardiff University in the U.K. – challenged the traditional views of Alzheimer’s disease by saying that “immunity is playing a significant role” in the disease.
Alzheimer’s disease is the sixth leading cause of death in the United States, affecting more than 5 million adults in the country.
The traditional view is that proteins accumulate in the brains of patients, leading to neuronal death. The culprits are the amyloid beta peptide and the tau protein.
Amyloid beta is produced when a short section of the amyloid precursor protein (APP) is severed. The function of the peptide in normal brain function is not known, but some evidence points toward a role in neurons. In Alzheimer’s disease, amyloid beta accumulates in plaques in the spaces between neurons.
Tau is a structural protein, important for neuronal function. But in Alzheimer’s, tau does not function properly and accumulates in tangles in neurons. How this contributes to cell death is unknown, but there is new evidence that shows that abnormal tau processing can lead to toxic effects.
How are scientists challenging the traditional view that abnormal protein buildup in the brain is to blame for the neurodegeneration seen in Alzheimer’s disease?
Joint efforts to identify new genetic variants
Until 2009, only four genes were known to be associated with Alzheimer’s disease. Mutations in three of these – APP, presenilin 1, and presenilin 2 – cause the inherited form of Alzheimer’s. This typically develops early in life, between the ages of 30 and 50. It is also known as early-onset Alzheimer’s disease.
Less than 1 percent of Alzheimer’s disease patients have this inherited form of the condition, in which an overproduction or abnormal folding of amyloid beta in the brain can be observed.
The majority of patients have the sporadic form of Alzheimer’s. Despite the fact that mutations in the apolipoprotein E gene (APOE) were known to be involved in susceptibility and earlier age of onset, only a subset of patients have the variant associated with the disease.
Predicting an individual’s risk of developing the disease with accuracy is, therefore, a challenge. For many years, there was a serious lack of progress in research looking to establish the underlying causes of susceptibility.
Today, we know that sporadic Alzheimer’s disease has a large genetic component, with its heritability being in the range of 58 to 79 percent. This means that other genetic variants must be involved.
Advances in genetics and technology led to a breakthrough, in 2009, that saw Prof. Williams and other researchers identify three new genes associated with Alzheimer’s disease using genome-wide association studies (GWAS).
Prof. Williams told the audience at the AAIC that it very quickly became clear that future discoveries using this type of genetic analysis would be dependent on data from large numbers of patients being available. To her, the only way to achieve this would be to collaborate with other teams around the world.
At the AAIC in 2010, held in Hawaii, the International Genomics of Alzheimer’s Project (IGAP) was born. IGAP is a collaboration of four large research consortia, led by Prof. Williams and other scientists across the U.S. and Europe.
IGAP researchers and other scientists have now identified 30 genes and genetic locations across the human genome that are involved a person’s susceptibility to Alzheimer’s. But what can scientists do with this new genetic information?
Identifying individuals at risk
In a study published in the journal Neurobiology of Aging in 2017, Prof. William’s team used their knowledge of susceptibility genes to test how accurately they could predict an individual’s risk of Alzheimer’s disease.
Using data from 17,000 Alzheimer’s patients and 37,000 controls, and looking at 87,583 mutations, they were able to identify the condition with an accuracy of 74.5 percent.
Prof. Williams explained that they were “now able to predict quite a lot of the risk of AD [Alzheimer’s disease] and it’s better than looking at APOE.”
“We have other genes that are protective and risk variants,” she added. Her team can use these to generate risk prediction scores. Knowing an individual’s risk level could help to identify who would benefit the most from early interventions.
But scientists still do not fully understand what causes the disease. Can these new genetic findings help?
From susceptibility to disease mechanism
Rather than looking at each of the susceptibility genes in isolation, Prof. Williams and her team are interested in the pathways that these genes are involved in.
The strongest association that they have been able to identify has been the immune pathway. Other cellular processes are also implicated to some extent, including cholesterol transport and protein folding.
“We find very little evidence of amyloid beta production affecting common AD,” Prof. Williams said, adding that they did find variants that affect amyloid beta processing and clearance.
So might the amyloid buildup seen in Alzheimer’s patients be less of a problem with excess production and more to do with other processes?
Prof. Williams challenged the audience to imagine a scenario wherein there was no historic knowledge of the genes implicated in amyloid processing being involved in Alzheimer’s disease. “Alzheimer’s disease is more of an autoinflammatory disease, than anything else,” Prof. Williams said.
“What we are seeing with immunity is happening quite early in the disease and maybe a primary event that is happening alongside amyloid [accumulation],” she added. “What we need to do is to understand mechanisms.”
The team’s latest discovery was published this week in Nature Genetics, and it supports this theory.
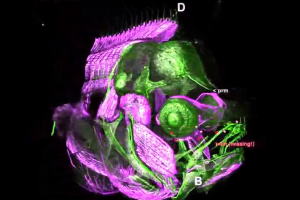
This study, performed by the IGAP group, identified two new genetic variants that confer Alzheimer’s disease risk. The genes – phospholipase C gamma and B-3-domain-containing transcription factor ABI3 – are highly expressed in microglial cells in the brain, which are part of the immune system.
Prof. Williams told the audience that scientists around the world are now studying genetic models to better understand how the immune system is involved in the neurodegeneration seen in Alzheimer’s.
What is really important is how researchers are putting this new knowledge and redefinition of the condition to use.
Pathways and drug targets
Prof. Williams explained that scientists can now take a more global view of the pathways involved in the disease. “We might find drugable targets, that might not be directly related to the genes,” she added.
Sir Simon Lovestone, a psychiatrist and professor of translational neuroscience at the University of Oxford in the U.K., echoed this sentiment in the plenary session at the AAIC that immediately followed Prof. Williams’s talk.
Prof. Lovestone’s team used datasets from patients across the U.K. and Europe to look at neurodegenerative diseases.
“I want to make a case, that we can use this data, real world data, electronic health record data, that we can accelerate the search for drugs in Alzheimer’s research,” he told the audience.
To illustrate his approach, he explained that by looking at large numbers of patients and performing GWAS studies, his team can identify “pathways associated with all diseases”.
This led them to identify shared immune pathways associated with Alzheimer’s disease, age-related macular degeneration, and diabetes.
Crucially, it allowed them to look at pathways, rather than individual genes, to identify points along those pathways in laboratory studies that can be targeted with drugs.
Advances in technology are arming scientists with an improved knowledge of the genetics that underpin Alzheimer’s disease and which molecular pathways are involved in the disease pathology.
How this knowledge will help patients remains to be seen, but new ideas are certainly pushing the frontiers of Alzheimer’s research and drug development.
Source: Medical News Today
Alzheimer’s disease is a progressive neurodegenerative disorder, thought to be caused by buildup of proteins in the brain. But there is increasing evidence that different biological processes are at the heart of the disease, providing scientists with a different approach to possible therapies.